Understanding Cardioversion and Heart Health
Cardioversion is a medical procedure used to restore a normal heart rhythm when the heart begins to beat irregularly or too quickly. Many people first encounter the term when they experience atrial fibrillation or atrial flutter, two of the most common rhythm disorders. These conditions can cause rapid, irregular heartbeats that lead to fatigue, dizziness, and even serious complications if left untreated. Because cardioversion is often recommended as an early treatment option, understanding how it works can help patients feel more confident and prepared. In this article, you will learn what cardioversion is, how the procedure is performed, what risks may be involved, and what to expect afterward. You will also discover how cardioversion compares to defibrillation and how to support long-term heart health following the procedure.

What Is the Cardioversion Procedure?
Cardioversion can be performed in two primary ways, and both are designed to restore a steady, healthy rhythm. Electrical cardioversion uses controlled electric shocks delivered through pads placed on the chest or back. These brief pulses reset the heart’s electrical system, allowing the normal rhythm to take over. Chemical cardioversion, on the other hand, uses medications to correct the rhythm. These drugs may be given intravenously or orally and work by stabilizing the electrical signals within the heart. Although the methods differ, both approaches aim for the same goal: a safe and effective return to normal cardiac function.
Patients typically undergo a preparation process before the procedure begins. Preparation often involves blood tests, imaging, and an evaluation of medications already being taken. In many cases, doctors recommend avoiding food or drink for several hours beforehand. For those with atrial fibrillation, anticoagulant medications may be prescribed in advance to reduce the risk of stroke during cardioversion. This step is crucial because an irregular heartbeat can allow blood clots to form, and restoring normal rhythm could potentially dislodge them. By identifying risk factors early, healthcare teams ensure the procedure is as safe as possible.
How Serious Is a Cardioversion Procedure?
Because it directly involves the heart, many people wonder how serious a cardioversion procedure truly is. While it is considered low risk, it is still a medical intervention that requires careful monitoring. Most patients experience only minor side effects such as temporary redness where the pads were placed or mild grogginess from sedation. More significant complications, though rare, may include arrhythmias that persist after the procedure, low blood pressure, or, in uncommon cases, stroke. The overall safety of cardioversion depends on several factors, including age, underlying heart conditions, and the presence of blood clots. When performed in a controlled medical environment, however, the procedure remains highly safe and successful for most individuals.
Can You Die During Cardioversion?
A common question patients ask is whether it is possible to die during cardioversion. While the thought is understandably alarming, the risk of death is extremely low. Life-threatening complications can occur, but medical teams take extensive precautions to prevent them. Continuous monitoring, sedation oversight, and the availability of emergency equipment all contribute to a high level of safety. Cardioversion may be avoided when a patient has an untreated clot, severe infection, or unstable heart conditions that require different types of care. By assessing each patient thoroughly beforehand, doctors ensure the procedure is only performed when it is the right option.
What Is Cardioversion vs Defibrillation?
Understanding the difference between cardioversion and defibrillation can also help clarify the purpose of each treatment. Cardioversion is used for controlled correction of specific arrhythmias, particularly atrial fibrillation and atrial flutter. It delivers a synchronized shock, meaning the electric pulse is carefully timed with the heart’s natural rhythm to avoid causing dangerous irregularities. Defibrillation, however, is an emergency procedure used when the heart goes into a life-threatening rhythm such as ventricular fibrillation. In this case, the shock is not synchronized because the heart’s electrical system has become chaotic and requires immediate reset. Knowing when each procedure is used helps patients understand why cardioversion is scheduled rather than performed in critical situations.
What Should You Not Do After Cardioversion?
After cardioversion, there are several important guidelines to follow. Immediately following the procedure, patients are usually advised not to drive or operate machinery, especially if they received sedation. Physical activity should be light for the first day or two, giving the body time to adjust to the restored rhythm. Medication compliance is essential. Many patients continue taking anticoagulants or rhythm-controlling medications to prevent recurrence. Activities such as drinking alcohol or consuming stimulants should be limited, as they can trigger irregular heart rhythms. Listening to the body and avoiding overexertion helps reduce the risk of complications.
Living With Your Heart Condition After Cardioversion
Maintaining a heart-healthy lifestyle after cardioversion is also critical. Some patients may require long-term modifications, including stress management, improved sleep habits, and careful monitoring of caffeine and alcohol intake. Triggers such as dehydration, smoking, and excessive exercise can also provoke irregular rhythms. Following medical advice, attending follow-up appointments, and tracking symptoms are important steps in supporting long-term heart stability. While cardioversion is effective, there is always the potential for recurrence, especially for those with underlying heart disease. By staying engaged in their care, patients increase their chances of lasting success.
Conclusion
Cardioversion is an effective medical intervention for restoring normal heart rhythm in patients with certain arrhythmias. While the procedure is quick and generally safe, it requires careful preparation, monitoring, and follow-up care. Understanding what cardioversion involves, including its benefits and limitations, empowers patients to make informed decisions about their cardiac care and work closely with their healthcare providers to maintain optimal heart health.
Take Action: Get Certified in Life-Saving Skills
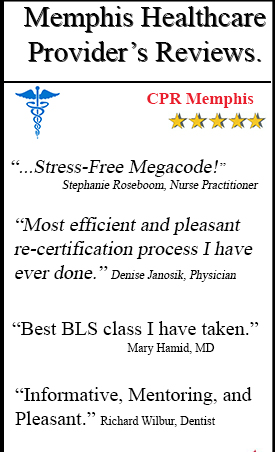
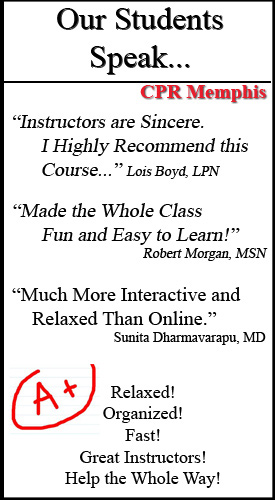
Understanding cardiac procedures like cardioversion reminds us how critical proper training is when responding to heart emergencies. Whether you’re a healthcare professional or simply want to be prepared to help in an emergency, CPR Memphis offers the comprehensive training you need.
CPR Memphis is an American Heart Association training site that offers initial certifications and renewal in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. All classes are stress-free and hands-on, ensuring you gain practical skills and confidence.
Don’t wait until an emergency happens—get your CPR certification in Memphis today or advance your skills with our ACLS classes in Memphis. Our expert instructors provide the quality training that could help you save a life. Visit CPR Memphis now to enroll in a class that fits your schedule and take the first step toward becoming someone’s hero.
FAQs About Cardioversion
Q1: How long does a cardioversion procedure take? A cardioversion procedure typically takes only 5 to 10 minutes to perform. However, you should plan to be at the hospital or medical facility for several hours. This includes time for preparation, where you’ll be connected to monitoring equipment and possibly given sedation, as well as recovery time afterward. Most patients are monitored for at least an hour after the procedure to ensure their heart rhythm remains stable before being discharged.
Q2: Is cardioversion painful? The procedure itself is not painful because patients are given sedation or light anesthesia beforehand. You’ll be asleep or in a deeply relaxed state during the electrical shock, so you won’t feel anything. Some patients report mild chest discomfort or skin irritation at the electrode sites afterward, similar to a sunburn sensation, but this typically resolves within a few days. The sedation also means you likely won’t remember the procedure itself.
Q3: What is the success rate of cardioversion? Cardioversion has a high immediate success rate, with about 90% of patients returning to normal sinus rhythm right after the procedure. However, maintaining that rhythm long-term varies by individual. Approximately 50% of patients remain in normal rhythm one year after the procedure. Success rates improve when cardioversion is combined with anti-arrhythmic medications and lifestyle modifications. Factors affecting long-term success include the duration of the arrhythmia before treatment, underlying heart conditions, and adherence to prescribed medications.