UNKNOWN LAB REPORT
Microbiology Unknown
Rachel Owens
Spring 2013
INTRODUCTION
Distinguishing between microbes is very significant. Knowing what agent is causing a disease can be vital for determining the accurate treatment for that particular disease. Equally important, is being aware of which microbes are favorable to have and important for homeostasis. The point of this study was to identify two unknown bacteria by employing all methods that had been used and learned about throughout the Microbiology Laboratory class.
MATERIALS AND METHODS
An unknown labeled 125 was handed out by the lab instructor along with the instructions to use the procedures from previous labs to determine the identity of two separate bacteria. Protocol from the course laboratory manual by McDonald et. al (1) was followed, unless otherwise noted.
Discovering the identity of the two unknown bacteria began with conducting an attempt to isolate a pure culture of each bacterium. A basic nutrient agar plate was the medium chosen for isolation and the isolation streak method described on page 10 in the lab manual was used in an effort to separate the unknowns. Succeeding the incubation period, the growth and morphology were observed and recorded. Two separate colonies had grown and the difference in appearance between the two different colonies was reason to perform a Gram stain on both bacteria to verify the existence of Gram positive and Gram negative bacteria. Also, two more nutrient agar plates were used to grow the isolated colonies separate from one another for quality control. The quality control bacteria were Gram stained as well as the unknown to confirm the Gram stain reaction was completed properly. The bacterium that was determined to be Gram negative rods will be further referred to as Unknown A, whereas the bacterium that was determined to be Gram positive cocci will be further referred to as Unknown B. There was an error and as a result, an alternate unknown bacterium was assigned and determined to be Gram positive rods. This alternate was labeled Alternate Number 8 and will further be referred to as Unknown C. Tests following the Gram staining have been chosen from the unknown identification tables handed out by the instructor.
Table 1 lists the test, purpose, reagents, and results.
The following biochemical tests were performed on Unknown A:
- Mannitol
- Urea
- Indole
- Citrate
The following biochemical tests were performed on Unknown C:
- Milk Agar
- Maltose
- Methyl Red
- Oxidase
RESULTS
TABLE 1. Unknown A
| Test | Purpose | Reagents | Observations | Results |
| Gram Stain | To determine the Gram
reaction of the bacterium |
Crystal violet,
Iodine, Alcohol, Safranin |
Pink Rods |
Gram Negative
rods |
| Mannitol | To determine the ability of
an organism to ferment mannitol |
Mannitol,
Phenol red |
Color change
from pink to yellow |
Positive for
acid production |
| Urea Test | To detect the enzyme
Urease |
Phenol red | No color change | Negative for
urease |
| Indole Test | To determine the ability of
the organism to split indole from the amino acid tryptophane |
Kovac’s Reagent
added to 1 ml of tryptone broth |
No red ring at top of broth |
Negative indole test |
| Citrate Test | To determine the ability of
an organism to use citrate as a sole source of carbon |
Sodium citrate
medium, ammonium phosphate, bromthymol blue |
Color change from
green to blue near surface |
Positive for
citrate permease |
TABLE 2. Unknown C
| Test | Purpose | Reagents | Observations | Results |
| Gram Stain | To determine the Gram reaction of the bacterium | Crystal Violet, Iodine, Alcohol, Safranin | Purple rods | Gram positive rods |
| Casease Test | To determine the ability of an organism to produce casease | Milk protein casein | No clearing around the area of growth | Negative for casease production |
| Maltose Test | To detect carbohydrate fermentation | Peptone, phenol red, maltose | Color change from red to yellow | Positive for carbohydrate fermentation |
| Oxidase Test | To determine the presence of cytochrome c | Oxidase paper | Purple / black color change | Positive oxidase test |
| Methyl Red | To determine the ability of an organism to ferment glucose | MRVP | After adding methyl red to 1 ml color changed from light yellow to red | Positive for production of acid from glucose fermentation |
DISCUSSION/CONCLUSION
Once the four different biochemical tests were complete, it was concluded that Unknown A of the Unknown #125 was Enterobacter aerogenes. A simple Nutrient Agar plate was used to grow the isolated bacterium for use of additional tests. Once a Gram stain concluded that Unknown A was Gram negative rods the pure culture was then inoculated onto a Mannitol Salt Agar plate. When, after incubation, the color of the agar changed from pink to yellow it was concluded that the Unknown A had Mannitol fermenters present because acid was produced. This result suggests that Unknown A was Esherichia coli, Klebsiella pneumonia, or Enterobacter aerogenes. Then, a Urea broth test was conducted. The results from this test were negative which means there was no production of urease to break down urea and produce a pH change to trigger the phenol red to turn pink. This outcome eliminated Klebsiella pneumonia as a candidate. Next, a tryptone broth tube was inoculated and incubated for the first steps in a test for Indole. Once Kovac’s reagent was added and the top of the broth did not turn a dark red, it was decided that this was a negative test for Indole. This indication concluded that the Unknown A was Enterobacter aerogenes. Finally, a Citrate test was executed for confirmation. Unknown A had a positive result meaning that is was able to use citrate as a sole source of carbon, confirming that the Unknown A was Enterobacter aerogenes.
Enterobacter aerogenes (E. aerogenes) is in the Enterobacteriaceae family (2). Most often, this bacterium resides in soil, water, dairy products and inhabits the natural flora in the gastrointestinal tract of animals as well as humans (3). E. aerogenes can cause urinary tract infections and hospital-aquired infections (3). The majority of the infections are etiologically due to inadvertent transfer of bacteria during surgery or prolonged treatment in hospitals in patients who use venous or urethral catheters. The genus Enterobacter is more specifically a opportunistic pathogen and is sought out to be one of the many key causes for intra-abdominal infections second to E. coli (3). Infections commonly attributed to E. aerogenes are respiratory, gastrointestinal, and urinary tract infections, specifically cystitis, in addition to wound, bloodstream, and central nervous system infections (1,2,3). Furthermore, E. cloacea and E. aerogenes are the species most commonly associated with adult cases of meningitis (2). The severity of these infections generate an importance to isolate, identify and test for susceptibility for the causes of these nosocomial infections.
References
- McDonald, V., Thoele, M., Salagiver, B., & Gero, S. (2011). Lab Manual for General Microbiology: Bio 203. N.p.: St. Louis Community College at Meramec.
- Fraser, Susan L (2012, Mar 11). Enterobacter Infections. In Medscape Reference. Retrieved from http://emedicine.medscape.com/article/216845-overview#aw2aab6b2b2
- Tortora, Funk, Case (2007). Microbiology an Introduction: San Francisco. Pearson Education Inc.
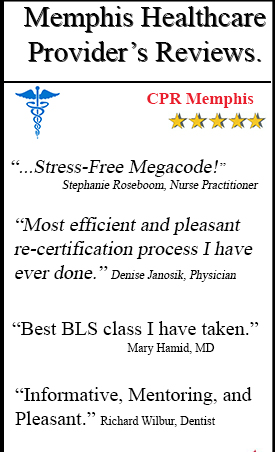
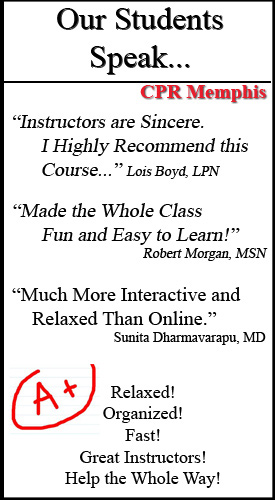
CPR Memphis offers CPR classes for healthcare providers, a.k.a. Basic Life Support for healthcare providers for nurses, doctors, dentists, radiologists, pharmacists, etc. For an American Heart Association certified class please call 901.438.4200