Cardiac arrest is one of the most critical emergencies a healthcare provider can face, and rapid, accurate rhythm recognition is key to patient survival. In these life-threatening situations, understanding the difference between shockable and non-shockable rhythms is essential. While shockable rhythms such as ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) require immediate defibrillation, non-shockable rhythms demand a different approach focused on high-quality CPR, medications, and identification of underlying causes. For healthcare providers, mastering these distinctions can mean the difference between life and death.

Understanding Cardiac Rhythms in Arrest Situations
What Are Non-Shockable Rhythms?
Non-shockable rhythms are cardiac rhythms observed during cardiac arrest that do not respond to defibrillation. They are characterized by electrical activity that is either absent or insufficient to produce effective cardiac output. Unlike shockable rhythms, which exhibit chaotic or rapid electrical activity, non-shockable rhythms indicate that the heart is unable to generate sufficient contractions to maintain circulation. This fundamental difference defines treatment priorities, making rhythm recognition an indispensable skill for providers in both hospital and pre-hospital settings.
Why They’re Called “Non-Shockable”
The term “non-shockable” arises from the fact that defibrillation is ineffective in restoring a viable rhythm. In shockable rhythms, electrical cardioversion can reset disorganized cardiac impulses, but in non-shockable rhythms, the problem lies not in chaotic electrical activity but in the heart’s inability to produce coordinated contractions. This can result from severe hypoxia, metabolic disturbances, or structural heart conditions. Understanding the underlying pathophysiology of non-shockable rhythms allows clinicians to prioritize interventions such as high-quality CPR and rapid correction of reversible causes.
Types of Non-Shockable Rhythms
The two primary non-shockable rhythms are asystole and pulseless electrical activity (PEA).
Asystole (Flatline)
Asystole, often referred to as a flatline, indicates a complete absence of electrical activity in the heart. On an ECG, asystole appears as a straight, flat line. Common causes include prolonged hypoxia, advanced cardiac disease, or severe electrolyte disturbances. Prognosis for asystole is generally poor, with survival rates remaining low despite aggressive resuscitation. Prompt initiation of CPR and treatment of any reversible underlying causes are critical for any chance of recovery.
Pulseless Electrical Activity (PEA)
Pulseless electrical activity is defined by the presence of organized electrical activity on an ECG without a corresponding pulse or effective cardiac output. Unlike asystole, the heart’s electrical system is active, but mechanical contraction fails. Common causes of PEA are often remembered using the H’s and T’s: hypovolemia, hypoxia, hydrogen ion imbalance (acidosis), hypo- or hyperkalemia, hypothermia, tension pneumothorax, cardiac tamponade, toxins, and thrombosis (pulmonary or coronary). Prognosis in PEA varies depending on the rapid identification and correction of these underlying conditions.
Recognizing Non-Shockable Rhythms
ECG Characteristics
Recognizing non-shockable rhythms requires careful ECG interpretation and quick assessment of the patient’s condition. On the monitor, asystole is visually distinct, while PEA can be more subtle, showing organized electrical activity without a palpable pulse. Common mistakes include confusing fine VFib with asystole or overlooking PEA due to subtle waveform activity. Assessment protocols emphasize checking for a pulse, confirming the rhythm, and making rapid decisions to initiate CPR without unnecessary delays.
Assessment Steps
High-quality CPR is the cornerstone of non-shockable rhythm management. Effective compressions maintain perfusion to vital organs while buying time to address reversible causes. Compressions should be performed at a depth of at least two inches in adults, at a rate of 100 to 120 per minute, and interruptions should be minimized. Proper hand placement, adequate chest recoil, and coordination among rescuers are crucial to optimize outcomes.
Treatment Approach for Non-Shockable Rhythms
Medication Administration
Medication administration is another vital component in managing non-shockable rhythms. Epinephrine is administered as soon as possible, typically every three to five minutes during resuscitation. Vasopressin may also be considered in certain situations, with careful attention to appropriate dosing and routes of administration. These medications support systemic perfusion and increase the likelihood of achieving return of spontaneous circulation (ROSC).
Advanced Airway Management
Advanced airway management should be considered when indicated, ensuring effective ventilation while avoiding hyperventilation, which can reduce coronary perfusion. Establishing an advanced airway enables continuous compressions while maintaining oxygenation and carbon dioxide removal, both of which are critical for patient survival.
Identifying and Treating Reversible Causes
Identifying and treating reversible causes is central to improving outcomes in non-shockable rhythms. The H’s and T’s provide a structured approach to uncover underlying issues such as hypovolemia, hypoxia, acidosis, electrolyte imbalances, hypothermia, tension pneumothorax, cardiac tamponade, toxins, and thrombosis. A systematic approach ensures that all potential contributors are evaluated and corrected promptly.
The ACLS Algorithm for Non-Shockable Rhythms
The ACLS algorithm for non-shockable rhythms guides healthcare providers through structured interventions. Initial assessment and CPR initiation are followed by rhythm checks at set intervals, medication administration, and continuous reassessment. Decisions to continue or terminate resuscitation are guided by factors such as duration of arrest, response to interventions, and adherence to current guidelines, with ethical considerations playing a critical role.
FAQs About Non-Shockable Rhythms
- Can you survive a non-shockable cardiac arrest? Yes, survival is possible with prompt and effective CPR. Non-shockable rhythms like PEA and asystole require immediate high-quality chest compressions and identification of reversible causes. While survival rates are generally lower than for shockable rhythms, quick recognition and proper treatment significantly improve outcomes. The key is starting CPR immediately and addressing underlying issues such as hypovolemia, hypoxia, or medication toxicity.
- What should I do if I encounter someone with a non-shockable rhythm? Begin CPR immediately with continuous chest compressions at a rate of 100-120 per minute. Call 911 or ensure someone else does. Continue CPR until advanced medical help arrives. Do not delay compressions waiting for an AED—if the rhythm is non-shockable, the AED will advise “no shock” and prompt you to continue CPR. Every second counts in maintaining blood flow to vital organs.
- How can I tell the difference between shockable and non-shockable rhythms without medical equipment? You cannot determine the specific rhythm without proper monitoring equipment. However, this shouldn’t delay your response. If someone is unresponsive and not breathing normally, begin CPR immediately. An AED will automatically analyze the rhythm and tell you whether a shock is advised. Your focus should be on providing high-quality CPR regardless of the underlying rhythm.
- Why is CPR training important for recognizing non-shockable rhythms? Proper CPR training teaches you how to respond effectively to all cardiac emergencies, including non-shockable rhythms. You’ll learn high-quality chest compression techniques, proper AED use, and how to recognize when defibrillation isn’t indicated. Training gives you the confidence to act quickly and correctly, which is critical since non-shockable rhythms require immediate, uninterrupted CPR to maximize survival chances.
Conclusion
Understanding non-shockable rhythms is crucial for anyone involved in emergency response. While PEA and asystole present more challenging scenarios than shockable rhythms, immediate high-quality CPR remains the cornerstone of treatment. Recognition that not all cardiac arrests require defibrillation helps responders focus on what matters most: maintaining circulation through effective chest compressions and identifying reversible causes. Whether you’re a healthcare provider or a concerned citizen, knowing how to respond to these life-threatening emergencies can make the difference between life and death.
Call to Action
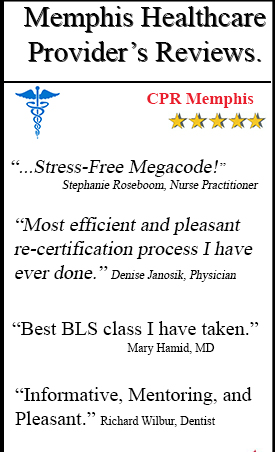
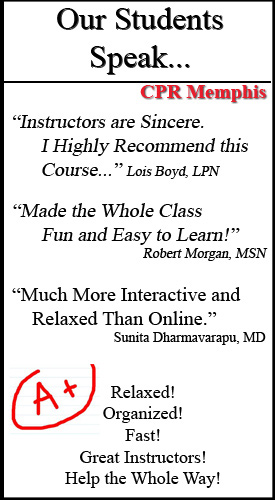
Don’t wait until an emergency happens to learn these life-saving skills. CPR Memphis, an American Heart Association training site, offers comprehensive CPR certification in Memphis and BLS classes in Memphis that cover both shockable and non-shockable cardiac rhythms. Our hands-on, stress-free courses include BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid certifications and renewals.
Equip yourself with the knowledge and confidence to respond effectively in any cardiac emergency. Enroll in a class today at CPR Memphis and become prepared to save a life tomorrow.